For most states with medical cannabis laws, patients are required to go through a screening process once a year to allow access to cannabis. On the one hand, this screening process is not designed to be severe, and realistically, few people are turned away from help with cannabis. On the other hand, this process is intended to serve as a boiler-plate to keep cannabis out of the hands of individuals for whom it might not be appropriate. Seeing that cannabis does not have harmful side-effects and is physically very safe, the real concern is whether patients who are already in an altered state of mind should be taking a psychoactive substance. Studies have linked early cannabis use to hastening the onset of serious psychiatric illnesses such as schizophrenia. This is not unique to cannabis and also true of any psychoactive substance. If someone is having a hard time navigating reality, taking a medicine or recreational drug that alters his/her mind-state even further may push him/her over the edge.
Despite this well-established fact, there are also many psychiatric patients that receive relief from cannabis and tend to do worse without it. The medical field has also shown increased interest in treating psychiatric illness with cannabis. So what’s the deal? Does cannabis contribute to or relieve schizophrenia? Or is there no effect? The difficulty in answering this lies partly in the fact that schizophrenia is not well understood and could actually be multiple illnesses that have been lumped into one category due to similar behaviors. These behaviors include “false beliefs, unclear thinking, auditory hallucinations, and failure to recognize what is real.” Certainly what is real is debatable (thanks Christopher Nolan), but for those of you suffering from the illness or for friends of those suffering, you know that there is a difference between someone questioning reality in a philosophical way and someone questioning reality in a tangible way that impairs basic functioning and/or increases their risk of death, pain or loss of freedom.
As is the case with a lot of psychiatric illnesses at this point in history, we don’t completely understand the brain circuits involved, and our pharmaceuticals are broad, rough tools that are mostly ineffective. Most (but not all) schizophrenic patients never get better, and they have a heart-breaking wrestle with the illness their entire lives, going on and off of different medications as needed. For this reason, the medical community is actively looking for new ways of dealing with psychotic illnesses. We’ve talked before on the blog about cannabidiol (CBD) and its calming effects, so readers should not be surprised that the interest over cannabis is predominantly about using CBD, not THC. THC constitutes most of the “high” part of medicating with cannabis, so while it is the focus of many recreational users, this is likely the component of cannabis that can tip psychiatric patients over the edge. CBD, however, has been shown to counter-act the high of THC, and as a result, researchers have speculated that CBD-only cannabis could be used to treat psychiatric conditions.
While more research is necessary, several findings seem promising. First, studies have confirmed that CBD can help improve mental deficits usually found in patients with schizophrenia. Several neuro-imaging studies, which observed brain-wave response to CBD administration in healthy patients, showed that CBD increased MMN (auditory mismatch negativity) as opposed to THC with CBD or simply nothing at all. MMN is known to be reduced in patients with schizophrenia, meaning that this is one sign CBD can help overcome some of the poor mental resource allocation of psychotic patients.
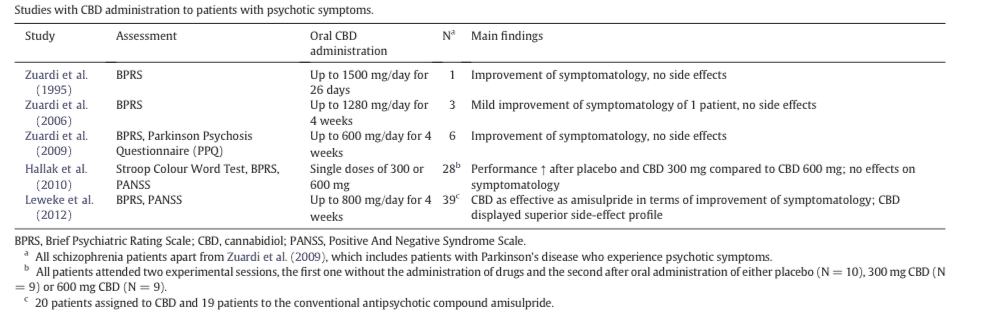
More importantly, however, are studies of CBD administration to patients with psychotic symptoms. Tabitha Iseger and Matthijs Bossong, working jointly from King’s College and Utretcht University Medical Center respectively, have compiled a list of those studies in the table below:
[table inset: Table listing five studies of CBD administration to patients with psychotic symptoms]
Hallak and Leweke, tested around 30 patients at a time with various doses of CBD (300-800 mg/day). For some patients, symptoms of psychosis improved, while for others, nothing occurred. Researchers also cannot rule out placebo effects, or effects stemming from patients believing they will get better. However, the positive news is that none of these experiments had harmful side-effects on patients. In experimenting with treating psychosis with CBD, we have yet to see the type of negative side-effects we see from the typical pharmaceutical approaches. This also seems to hint at the answer to the question of this blog post, which was whether cannabis contributes to or improves schizophrenia. At this time, leaving THC out of the equation, we can feel fairly confident in saying that CBD improves or at worst does nothing for individuals with schizophrenia. Given that multiple causes likely exist for the one illness known as “schizophrenia”, this could be because CBD is only effective for some forms of schizophrenia and not others.
Final conclusion: it would be our recommendation that those with psychiatric disorders who already use cannabis steer clear of high-THC strains for the time-being and explore high-CBD strains. However, this is still something that seriously ill patients must discuss with their long-term doctors, as correctly treating psychiatric illness requires knowing treatment history and building somewhat of a treatment “relationship” with a doctor or caregiver.
Works Cited
Tabitha Iseger, Matthijs Bossong. (2014) A systematic review of the antipsychotic properties of cannabidiol in humans. Schizophrenia Research (2015) 162:153-161.