After years of negative propaganda from uninformed politicians, it is tempting to jump at evidence indicating cannabis could miraculously cure cancer. In fact, even well educated members of the cannabis community may tout this point as a reason for legalization. This mistake is understandable; the person may have read a report showing cannabinoids capable of killing tumor cells. The problem is that saying “CANNABIS CURES CANCER” without additional information is like saying, “MONEY CURES POVERTY”. Either statement could technically be argued to be true, but both statements are such reductive, simplistic views that they are entirely misleading on their own and actually very unhelpful to genuine progress.
The truth is that smoking cannabis or using topical cannabis extract almost certainly has no impact on preventing or curing cancer. Where the real progress is happening involving cannabis and cancer actually rests in the consideration of the endocannabinoid (eCB) system as a chemotherapy target. Currently, many different types of drugs are used as chemotherapy agents. Unfortunately, a lot of these drugs also exhibit friendly fire and kill non-cancerous cells or deplete other body resources to the extent that the process of chemotherapy is arduous and difficult for the patient. As a result, doctors must carefully aim to give patients as much chemotherapy as they can safely accommodate and no more. The eCB system and cannabinoids show promise as new chemo drugs, because they exhibit anti-tumor properties while at the same time are very gentle and natural to the human body. Currently, many different organizations are pursuing this line of thought, and as a result, readers can expect to hear more areas in which eCB system targeting can be effective against cancer growth and spread. However, for this article, we will consider papers involving melanoma, or cancer of the skin.
Melanoma is a particularly frustrating cancer to cure. Although chemotherapy regimens are available, they are mostly ineffective. The best solution currently available is early-detection and surgery to directly remove tumors. For this reason, Complutense University and Spain’s National Center of Oncology Research decided to do a comprehensive investigation of using cannabinoid receptors in the body to fight melanoma in both cell cultures and live rodents. To begin, researchers first confirmed the existence of both cannabinoid receptors, CB1 and CB2, in cancerous melanoma cells, using a wide variety of melanoma cell lines, which are grown specifically for researching cancer, as well as actual tumors. All cell lines exhibited both cannabinoid receptors, and of 61 tumors, only five lacked either receptor, with 36 having both. In other words, cannabinoid receptors are commonly found in melanoma cells. Having confirmed this, researchers moved on to applying cannabinoid receptor activators to cancerous and non-cancerous cell cultures and then measuring the number of live cells as a function of time.
The results are seen below:
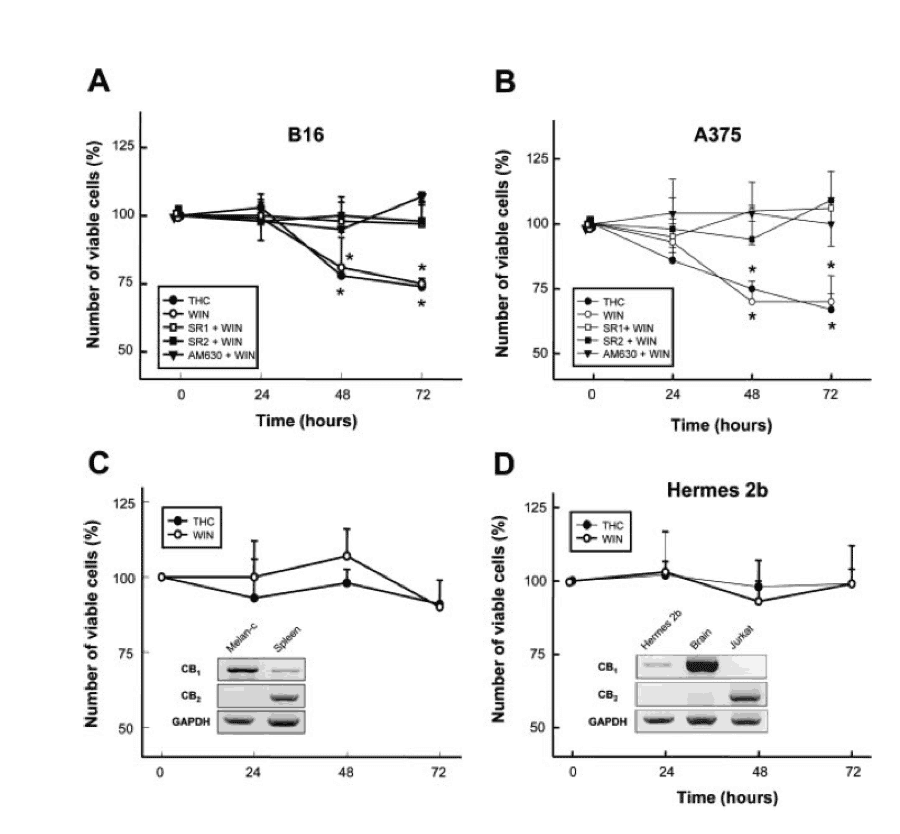
[Inset for graph: Graph showing the number of live cells in cancerous cell lines (top) and healthy cell lines (bottom) as a function of time from application of various chemicals.]
As shown in the top two graphs, which show melanoma cell lines B16 and A375, applying THC or WIN-55, 212-2 both lead to dramatic decreases in live cells. THC is, of course, the primary psychoactive cannabinoid in cannabis, whereas WIN-55, 212-2 is an artificial cannabinoid made synthetically. In the bottom two graphs, we see the results of applying the same chemicals to healthy, non-cancerous cell lines melan-C and Hermes 2b, which are healthy skin cells from mice and humans respectively. Notice that virtually no change occurs in healthy cells, meaning that THC and WIN-55, 212-2 both appear capable of targeting only cancer cells.
Following this experiment, researchers then moved on to investigating the effect of WIN-55, 212-2 and another cannabinoid receptor activator, JWH-133, by injecting them outside of the skin cell tumors growing in mice. To account for tumor-size differences, researchers measured tumor volume as a percentage of the original tumor volume and then averaged the results for each test group (nothing added, WIN added, and JWH added), which were then expressed in graph A below.
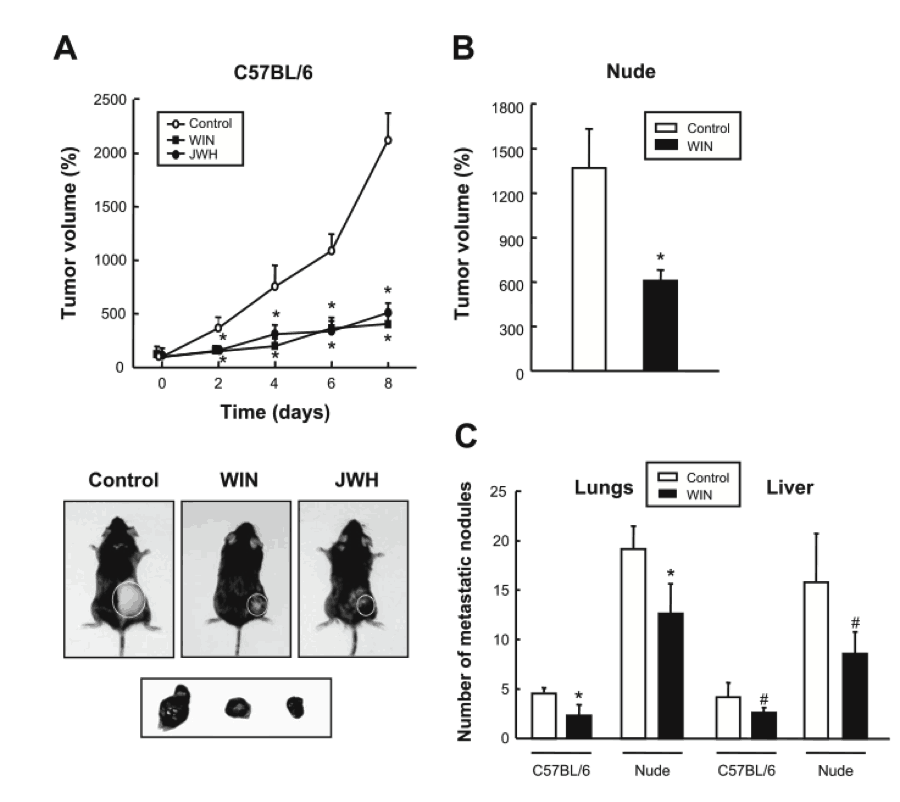
[Inset for graph: Graphs showing the tumor volume as a function of time with and without cannabinoids injected (top). Graph showing the number of cancer cell nodes in the lungs and liver for both normal mice and mice without immune systems with and without WIN added.]
As seen, while these injections did not completely halt tumor growth, both WIN and JWH significantly dampened growth almost identically to the previous cell culture experiments. At this point researchers could not be completely sure that the effects achieved were due entirely to cannabinoid receptor activation or if the immune systems of mice were also being triggered by the injected cannabinoids and playing a side role. To rule this possibility out, researchers performed a test of WIN injections on “nude” mice, which are mice without working immune systems. As seen in graph B, the dampening effect on tumor growth occurred even without the immune systems’ involvement, meaning that the effect is likely coming exclusively from cannabinoid receptor activation.
Finally, as seen in graph C, researchers measured the number of “metastatic nodules” found in other areas of mice with skin cancer tumors, both with and without WIN injections. Metastatic nodules are areas in which the skin cancer cells have migrated through the body via the blood or another pathway and have established a new colony of cancer cells. This specific action is what makes cancer life-threatening, since death occurs when cancer spreads to vital organs and causes them to fail. As seen in the graph, the number of new cancer growth sites in the lungs and livers of mice injected with WIN displayed a small but significant decrease, indicating that activation of cannabinoid receptors can limit melanoma cancer cell migration. This research is augmented by that of the Institute of Biophysics in Hungary, which performed an experiment earlier this year showing that CB2 receptor activation can inhibit or slow down the migration of melanoma cells through the blood-brain barrier.
Taken all together, this research shows tremendous promise for CB receptor agonists being developed as chemotherapy agents. Although THC and WIN-55, 212-2 will most likely not be the endpoint drugs adopted, it is safe to guess that they will provide suggestions for molecules that will eventually enter the realm of chemotherapy. At the very least, scientists are now becoming aware that the endocannabinoid system has a means of controlling cancer cell growth, that thus far has been all but ignored as a possible tool for fighting cancer.
Works Cited:
Cristina Blazquez, Arkaitz Carracedo, Lucia Barrado, et. al. (2006) Cannabinoid receptors as novel targets for the treatment of melanoma. The Journal of the Federation of American Societies for Experimental Biology (FASEB) (2006) 20:2633-2635.
Janos Hasko, Csilla Fazakas, Judit Molnar, et. al. (2014) CB2 Receptor Activation Inhibits Melanoma Cell Transmigration through the Blood-Brain Barrier. International Journal of Molecular Sciences (2014) 15:8063-8074.

