Today we’re revisiting a topic: the use of the endocannabinoid system as a possible therapeutic target for cancer treatment. Last time, we discussed the ability of some cannabinoid molecules to trigger cell death in cancerous cells. In that article we were careful to note that those results did not necessarily equate to a cancer solution and more testing would need to be conducted. Since then, cancer research has continued to be a focal point of the endocannabinoid research community, so we’re pleased to be able to further the discussion.
The leading cause of global cancer death is hepatocellular carcinoma (HCC). HCC is the most common type of liver cancer and usually brought on by other illness or stress, such as viral infection or alcoholism. The survival rate is generally poor, as by the time tumors are noticed, they are generally too big to remove. In fact, liver transplant is usually the most effective approach. Unfortunately, livers have a waiting list and most cases of HCC occur in undeveloped countries where some sort of solution is desperately needed. At this point in time, researchers are testing all sorts of new chemicals and processes. Endocannabinoids, with receptors all along the immune system, represent a unique approach to a solution
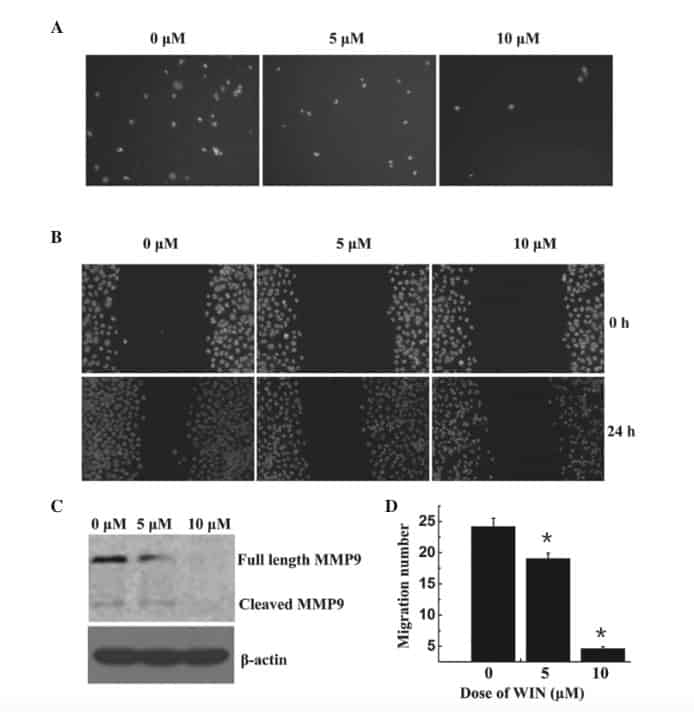
In earlier studies, the chemical WIN55,212-2 (WIN55), a synthetic cannabinoid which produces effects similar to the THC found in cannabis, has been shown to cause cell cycle arrest in the cancer cell line BEL7402 (carcinoma cells). Like THC, WIN55 actives CB1 receptors. Researchers at Guangzhou Medical University set out to re-confirm these results, as well as to delve deeper into why the cell cycle arrest is occurring. To do this, researchers transferred known concentrations of the carcinoma cell line into multiple-well plates and allowed the cells to settle and adhere to the container. Twenty-four hours later, they were treated with WIN55 at 0, 5, 10, and sometimes also 20 micromolar concentrations. Each culture was then dyed for an easier cell count and allowed to incubate for 1 hour at a warm temperature (almost 100 degress Fahrenheit). From there, multiple tests were carried out on the cells. First, researchers set out to discover the status of cells, dead or alive, as well as the reproduction rate. Secondly, researchers set out to test cell migration, which mimics/investigates how these cancerous cells could move throughout the body. Finally, researchers investigated at what stage of the cell life cycle cells were at when harvested.
The results confirmed previous experiments. DNA cell cycle analysis showed a greater percentage of cells currently on the G1 phase in response to an increase in WIN55 treatment (meaning many had stopped at that phase as a result of treatment). This was no surprise. Researchers took the experiment a step further when they tested the effects of WIN55 on the regulatory molecules that operate in that particular phase of the cell cycle, in order to see what WIN55 changed. In these studies, a decrease in the generation of the protein p27 was detected following WIN55 treatment. Since that in turn regulates the generation of proteins cyclin D1 and Cdk4, they were also investigated and found to decrease with treatment of WIN55. Without getting too deep into biology, this just means that we understand the specific pathway through which cells are arresting/ceasing to reproduce.
Besides failing to reproduce, cells began to stop migrating. According to migration testing, and as seen here in A and D of the table below, an increased dose of WIN55 led to a steep decrease in cell migration (close to an 80% decrease at 10 micromolar concentration, likely more at greater amounts).
What this means is that in lab conditions, cancer cells are left to die under the presence of WIN55. In theory, a cancerous tumor, a mass of cancer cells growing and migrating, would therefore be frozen and sent into remission. Additionally, WIN55 has been shown to be non-toxic to non-cancerous cells, which would indicate that it could therefore be a perfect anti-cancer target. Why would this occur? How could WIN55 have such a profound effect exclusively on cancer cells? Apparently, carcinoma cells have higher levels of CB2 receptors, making them more receptive to cannabinoid signaling. Although WIN55 predominantly targets CB1 receptors, researchers were able to confirm effects occurring through CB2 receptors (via applying CB2 antagonists to shut off the receptors in one study and noticing a decreased effect of WIN55).
This is not in itself a cancer solution, but the chances of this leading to a novel cancer treatment are reasonably high. Ironically, it seems that over-zealous cannabis activists who claimed cannabis could cure cancer were not as far off as scientists originally presumed! What we desperately need now are tests on cancerous tissues (i.e. tests that more closely mimic cancer spread within the human body). These tests will be even more predictive of the therapeutic potential of cannabinoids in treating cancer. Fortunately with the growing body of cell line research, these tests should not be far off.
Works Cited
Dacai Xu, Jianglin Wang, et al. (2014) Cannabinoid WIN55,212-2 induces cell cycle arrest and inhibits the proliferation of migration of human BEL7402 hepatocellular carinoma cells. Molecular Medicine Reports (2015) 12:7963-7970.

