Chances are that you or someone you know has been diagnosed with Attention-Deficit Hyperactivity Disorder (ADHD). ADHD is one of the most commonly diagnosed neurological conditions as well as one of the most controversial due to the difficulty of treatment and diagnosis. New research has begun to suggest that the body’s cannabinoid system, specifically cannabinoid agonists like those found in cannabis, may play a role in treatment.
In the Diagnostic and Statistical Manual of Mental Disorders, which is widely used as a diagnosis guide for doctors, ADHD is identified by a patient with measured trouble with mental functions that leads to inattention and hyperactivity. Unfortunately, what constitutes ADHD is therefore automatically open to a wide interpretation; at this point in time, our model of “attention” itself is incomplete. That’s not to say we don’t have some idea of the main chemicals that regulate consciousness. Norepinephrine is most responsible for vigilant concentration in the brain, and dopamine is most responsible for cognitive alertness. Moreover, many individuals with ADHD have thinner brain tissue in certain areas that regulate impulsivity. However, as research continues, the medical community is split over whether ADHD is even one illness. Many have proposed that the attention-deficit and hyperactivity symptoms stem from two different sources and as a result require different solutions.
However, what makes ADHD treatment most controversial is the use of stimulants for treatment. Ritalin was the first major drug to be prescribed for ADHD, but second and third-generation stimulants with longer effects and less tolerance, such as Adderall and Vyvanse, have now supplanted Ritalin. These drugs vary some, but all are stimulants designed to increase the dopamine and norepinephrine available to the brain. In some cases, these substances may be incredibly effective at solving the issues experienced by the patient. In other cases, doctors may be giving patients uneeded stimulants, which not only puts excess stress on the body but can also lead to devastating side-effects, such as hallucinations, slowed growth, insomnia, and circulatory system problems. As a result, the medical community has often discussed the over-diagnosis of ADHD, and the disorder in itself has become a cultural touchstone of a nation deeply attached to big pharmaceutical companies.
Recently, some research has indicated that the endocannabinoid system may play a role in the treatment of ADHD. One research group from Italy chose to specifically focus on testing impulsivity by comparing the behavior of spontaneously hypertensive rats (SHR’s) with normally developing Wistar-Kyoto rats. Spontaneously hypertensive rats have been accepted as a rat model of ADHD, so the research group was essentially attempting to compare ADHD vs. non-ADHD rats. To test impulsivity, researchers created a chamber with two nose-poking holes. The first delivered one pellet of food immediately upon a rat poking its head through, while the other delivered five pellets of food after an initial delay. When the delay is short, rats should naturally prefer the nose-poking hole that delivers more food. However, as the delay increases in time, the more impatient rats switch to the smaller, immediate hole, preferring a more immediate pay-off. Upon activating either hole, a time-out period would occur to prevent rodents from activating both, which forced rodents to “choose” between the two holes. After acclimating rats to the chamber, researchers slowly increased the delay time on the larger food delivery hole then recorded the percentage of time rats chose the delayed option. With this data, researchers were able to measure impulsivity, as the more impulsive rats transferred to the no-delay chamber much more quickly than rats with greater impulse control.
From this experiment, researchers observed several interesting phenomenona. First, SHR’s (ADHD rats) displayed a much higher variability in behavior than the “normal” WKY rats, which seemed to perform almost identically within their group. This seems to mimic ADHD in humans since a wide range of behaviors exists when comparing individuals with ADHD. Specifically, two sub-groups of the SHR’s were identified by splitting rats above the median impulse control and those below it. These groups could represent the split in ADHD patients between those with predominant attention issues and those with predominant hyperactivity issues. However, the juiciest finding occurred after the experiment when researchers dissected the rodent brains to measure receptor density in various areas. At this time, researchers observed that SHR’s had lower CB1 cannabinoid receptor densities in pre-frontal cortex regions than their WKY rat (normal rat) counter-parts.
This finding triggered an important question: if impulsivity is associated with a lack of density in CB1 receptors, could increasing the amount of cannabinoids that bind to those receptors make up for that lack of density and therefore reverse some of the impulsivity? To test this, researchers conducted several other experiments, one in which WIN-55,212, a chemical that binds to CB1 receptors like THC from cannabis, was given to some rodents, while an empty, “control” injection was given to the rest. The results are shown in the graph below.
Percentage of self-control of WKY and SHR strain rats with and without WIN cannabinoid agonist: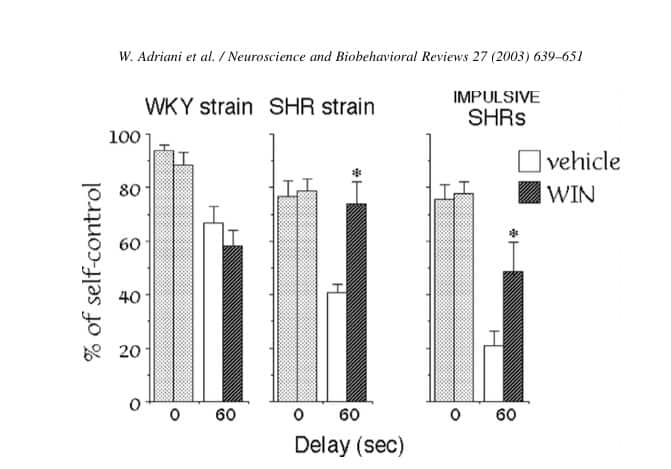
As the graph shows, while WIN slightly reduced impulse control in “normal” WKY rats, it significantly improved impulse-control in both groups of impulsive SHR rats. In the case of the most impulsive SHR rat group, WIN effectively doubled impulse control!
Should these results be duplicated in human trials, the implication would be that cannabinoid agonists could substantially improve impulse control in those with ADHD. This would mean that cannabinoid agonists could be used to replace or decrease the amount of prescribed stimulants in some cases of ADHD, which would result in a host of other positive health benefits and also decrease the harm of over-diagnosis of the disease. As always, rodent tests are not necessarily representative of human tests, so we will have to wait for this line of research to advance to human trials before drawing firm conclusions. Regardless, what we are seeing now is a strong indication that the cannabinoid system is involved in some way with ADHD. Readers can add that to the ever-growing list of brain functions and conditions that are mediated by the body’s cannabinoid system.
Works Cited
Walter Adriani, Antonio Caprioli, Oleg Granstrem, et. al. (2003) “The spontaneously hypertensive-rat as an animal model of ADHD: evidence for impulsive and non-impulsive subpopulations”. Neuroscience and Biobehavioral Reviews (2003) 27:639-651.

