by idgadvertisingold | Jun 26, 2018 | Medicine, Science
One of the recurring themes in Cornerstone Blog articles is the idea that cannabis can achieve some of the results of pharmaceutical drugs with less risk to health and financial cost. Opioids, for instance, are often seen as the last line of defense in treating pain,...
by idgadvertisingold | Aug 22, 2016 | Endocannabinoid System, Medicine, Science
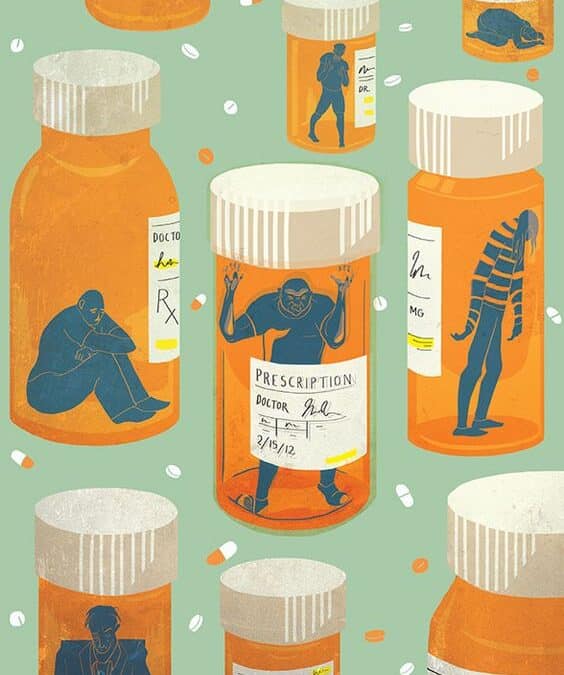
Opioids/opiates have provided significant and sometimes life-saving relief to countless patients. They remain some of the strongest painkillers available and can be especially helpful in rendering comfort in otherwise extremely painful terminal illnesses. Opioids work...

by idgadvertisingold | Feb 9, 2015 | Medicine, Science
The last time we spoke of opioids and cannabis, it was in reference to whether cannabis could interfere with opioid withdrawal recovery (spoiler alert: not observed). However, equally worth considering is the opposite end of the spectrum of opioid users: legitimate...
by idgadvertisingold | Aug 22, 2014 | Medicine, Science
The cultural perception of cannabis as a recreational narcotic is one reason many patients are not open to the option of cannabis treatment. As more states begin to offer medicinal cannabis, this cultural perception has largely reversed and enabled genuine research...